What is Apolipoprotein B and why is it important?
Atherosclerosis is the disease process that causes coronary artery disease. It is not a new condition. It has been found in 4000-year-old Egyptian mummies. In modern medicine, cholesterol is often described as being either good or bad. However, cholesterol is only ‘bad’ when it is in the wall of the artery. But how does it get there? And what makes it stay in the wall of an artery and cause a problem? Many things carry cholesterol around the body including HDL (often referred to as the good cholesterol) and red blood cells. Indeed, red blood cells carry a similar amount of cholesterol around the body as LDL particles (often referred to as the bad cholesterol).
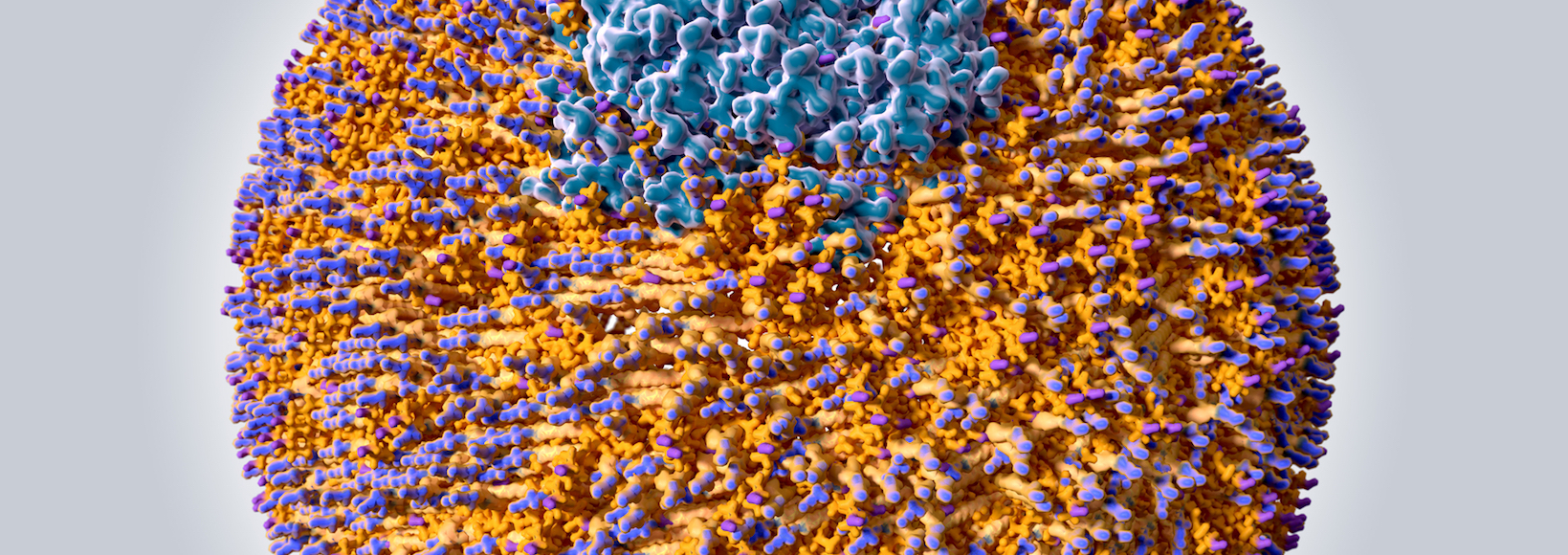
So what is it that makes LDL bad? Or to put it another way, how does good cholesterol turn bad? The answer is Apolipoprotein B. If you look at the picture of an LDL particle such as the one above, you can see what it is made of. Fat is not soluble in water, so in the bloodstream, it must be transported in a packaged group. Each LDL particle consists of one Apolipoprotein B (ApoB), which organises other proteins, lots of cholesterol molecules and a core of polyunsaturated fatty acids. Think of each LDL as being like a group of tourists in a strange city being guided by a tour guide, the ApoB.
It is not only LDL that ApoB is present on. There is also one ApoB molecule on each intermediate-density lipoprotein (IDL), very low-density lipoprotein (VLDL) and chylomicrons. Indeed all of these particles also have the ability to cause cardiovascular disease (CVD). This is why a measure of all of these atherogenic particles, referred to as non-HDL cholesterol, is thought to be a better marker of cardiovascular disease risk than alone.
The role of ApoB in atherogenesis, that is, the formation of atherosclerosis, is described by the “response to retention” hypothesis. Think of the artery as a road. The parts of the arteries that tend to have the most atherosclerosis are busy junctions. In cities the world over, busy junctions are often the sites of groups of bars and restaurants. Imagine now our group of tourists, the group of cholesterols with their ApoB guide wandering around the city. Imagine further that our group of tourists isn’t just any group of tourists but that they are a stag-do. Now a stag-do, our group of cholesterols, wants to find the busiest bar to go into. So it’s ApoB tour guide takes them to a bar at one of the busiest junctions and gets them in past the bouncer at the door.
Once inside the bar, the owner wants to keep this group in so that they continue to spend their cash in there. The artery lining acts in a similar way. But ultimately, acting in this way is going to be unhelpful for both the bar and the artery lining. How does the bar owner keep the group in the bar? Of course, by putting on the football, giving the tour guide a free drink and starting a happy hour. The artery lining acts, in the same way, to keep the LDL in the bar. Lipoprotein lipase and secretory sphingomyelinase are enzymes in the arterial wall that aid the retention of the ApoB and its cholesterol particles there. In the bar, as it’s getting busier and the punters are getting drunker our stag-do is swallowed up in the melee and drinks are being spilt everywhere. In the arterial lining, the ApoB and its cholesterols get swallowed up by macrophages (white cells) creating foam cells. Everyone in the bar is getting very merry, the atmosphere is really getting going, drinks are flying, people are up on the bar and more punters want to join the action. In the arterial lining, enzyme activation causes more retention of atherogenic particles. And it’s just then that the trouble really starts. As drinks and elbows start to fly and things get heated and people start to push past each other. First, a bottle smashes the window and then someone falls through the fire escape and everyone spills onto the street. The police are called. The area is blocked off. In the artery, the macrophages make enzymes that weaken the overlying cap and also release tissue factor. This agent is prothrombotic, it causes clots to form. It is the equivalent of calling the cops. Patry’s over. The artery is blocked.
So which is better at determining the risk of cardiovascular disease, non-HDL (which reflects the mass of cholesterol) or ApoB (which reflects the number of atherogenic particles)? To determine this requires studies of discordance. These studies show that when non-HDL was high but ApoB was normal, CVD risk was not high. But when non-HDL was normal and ApoB was high, CVD risk was high. Thus ApoB is a superior measure of CVD risk.
So, we know that ApoB causes heart disease. New studies using a technique called Mendelian Randomisation have demonstrated that ApoB is implicated not only in heart disease but in stroke and diabetes. This type of study has also demonstrated that ApoB is associated with a significant reduction in lifespan. MR is a type of statistical analysis that uses variations in our genes to determine whether a certain exposure leads to a certain outcome. The fantastic thing about these studies is that confounding variables are removed. So, Mandellion Randomisation is excellent at establishing causality. In contrast, in an observational study causality can be difficult to determine because of confounding factors. A confounding factor is a variable that a study does not account for. An example of this would be a study looking at the link between heart disease and obesity that failed to take into account other important confounders such as age and smoking. Mendelian randomisation also eliminates reverse causality. This is a feature of observational studies when it can be difficult to ascertain what is the cause and what is the effect. An example of this would be does smoking cause lung cancer or does lung cancer cause smoking?
So when should we be measuring ApoB? The American Heart Association 2018 guideline on cholesterol management suggests that for people at intermediate risk of heart disease (risk between 7.5% and 20% on conventional risk scores) ApoB measurement can refine the selection of people at the highest risk. The 2019 European Society of Cardiology and the European Atherosclerosis Guidelines suggest that ApoB is the most accurate measure of CVD risk and a more accurate measure of lipid-lowering treatments. I mentioned previously the potential discordance between non-HDL and Apo-B. This is most common in people who are overweight, diabetic or have high blood values of triglycerides. These people should certainly have ApoB measured. However, atherosclerosis plaques grow over time. With the passage of time, more ApoB-containing particles are retained in the artery wall. So it is not just the number of ApoB-containing particles but the duration of exposure to them that is important. Therefore, it’s important to maintain low ApoB levels throughout life and start screening with ApoB early.
Dr J Hugh Coyne
Parsons Green