Breast Cancer: A Doctor's Guide
Inherited Risk, Prevention, Genetic Testing, Early Detection & Screening Explained
What Everyone Needs To Know About Breast Cancer
Breast cancer is the most common invasive cancer in the UK. It affects 1 in 7 women over their lifetime, with approximately 150 new cases detected daily. Treatments are getting better all the time, but it is still the second most common cause of death due to cancer in women.
We can also be aware of other risk factors which can increase or decrease the risk of breast cancer. We can also use the latest science in screening to check for genetic or inherited cancer risks, plus how to optimise your early detection of cancer.
❓ What Causes Breast Cancer?
No single thing causes breast cancer. Even people with a strong inherited chance of cancer can reduce their risk by knowing about other risk factors. Knowing about things in your lifestyle, family history and hormones which can increase your risk will help you stay healthy. Some of the key risk factors include:
🧬 Genetic & Hormonal Factors:
- Family history – Having a first-degree relative (for example a mother or sister) with breast cancer doubles your risk of developing breast cancer.
- Inherited gene mutations – Mutations in genes like BRCA1, BRCA2, and PALB2 increase the likelihood of developing breast cancer.
- Early menstruation or late menopause – When periods start at an earlier age, or carry on for longer it means your breast tissue will be exposed to more oestrogen over the year. This can increase the risk of breast cancer.
Hormone replacement therapy (HRT) – There has been lots of alarming news stories and conflicting evidence about the risk of breast cancer in recent decades. Fortunately, we now have very good scientific of how HRT affects the risk of breast cancer. Combined HRT does generally slightly increase the risk of a breast cancer diagnosis. The estimate is an extra 10 cases if 1000 women aged 50 to 59 used HRT for up to 14 years. So that is a true increase but it is very small. ‘Combined HRT’ means taking two hormones oestrogen and progesterone. We now have a new type of progesterone, called Utrogestan. This is a special type of progesterone which is made to be identical to the body’s natural progesterone. The extra risk of breast cancer from taking Utrogestan is estimated to be close to zero, for women taking HRT first the first 5 years in their 50’s. Women who no longer have a uterus (womb) do not need to take any progesterone with their HRT, they can take oestrogen alone. Oestrogen-only HRT is not thought to have any extra breast cancer risk. If you are worried about the risk of breast cancer from taking HRT it is sensible to look at all your risk factors before making a decision.
🍏 Lifestyle Factors:
- Alcohol – Just two units of alcohol per day, such as a single glass of wine, increases risk by 9%. This is a much bigger increase than HRT for instance.
- Obesity – Being overweight after menopause raises the risk of breast cancer, because having more adipose tissue (fat cells) means your body will have more oestrogen in the blood.
- Weight carried around the tummy is especially important. You can estimate this measuring your waist, or get an MRI to measure visceral fat.
- Physical inactivity – Regular exercise, like brisk walking 30 min/day for 5 days a week can lower breast cancer risk by up to 12%.
- Smoking – Current smokers have about 10% extra risk compared to people who have never smoked.
- Previous Radiotherapy – You may need extra screening, if you’re not sure check with your GP.
- Having children – Women who have had children are at lower risk than those who have never had a baby. Starting a family at a younger age also seemed to be more protective in studies. Breastfeeding also seems to be protective, this is probably because it often delays periods restarting, and having few periods reduces the risk of breast cancer.

👀 Watch For Breast Cancer Symptoms:
Having these symptoms doesn’t always mean you have breast cancer, but it’s still important to find out what’s causing them.
Don’t delay in making an appointment with a GP to talk about your symptoms.
- A lump or swelling in the breast, upper chest or armpit
- A change to the skin, such as puckering or dimpling
- A change in the colour of the breast – the breast may look darker, red or inflamed
- A nipple change, for example it has become pulled in (inverted)
- Rash or crusting around the nipple
- Unusual liquid (discharge) from either nipple
- Changes in size or shape of the breast
🩻 How Can You Detect Breast Cancer Early?
Screening Options Explained
Currently, less than 40% of breast cancers are diagnosed at stage 1. It is important to diagnose breast cancer early as survival for people diagnosed at stage 1 is over 98% at 5 years.
NHS Breast Screening in the UK
A mammogram is a type of scan of the breast tissue. It uses x-rays to take a ‘picture’ of the breast tissue, looking for cancers. Many of these cancers can not be felt, they are only visible on the mammogram.
NHS Screening
- Females aged 50 to 71 years of age will be invited every 3 years for a screening mammogram.
- If you think you have missed a check-up then find out your local NHS breast screening centre online here and get in touch today.
High-Risk Screening
- People who are found to have an increased risk, for example, because of a family history of breast cancer, may be offered screening earlier by their local breast clinic. For instance, they may be offered mammograms starting earlier at 40 years of age.
Very High-Risk Breast Screening
- People who have a harmful genetic variant such as a BRCA1 mutation, or have had radiotherapy for lymphoma, will be invited by the NHS for extra screening. This is commonly a mammogram plus a breast MRI scan every year from 30 to 50 years of age.
- Women can only be referred to this screening programme with their results by a genetic or breast cancer hospital specialist.
Why 40 Is The New 50 In Breast Screening
The UK breast screening programme starts at a later age than nearly all other countries. There is excellent evidence that screening younger women more frequently can save lives.
Screening women every year from 40 onwards can reduce the risk of dying from breast cancer by 25% in just 10 years. That’s why an annual mammogram screening over 40 years is always part of our health screenings at Coyne Medical
What about false alarms? False positives or false ‘alarms’ happen with all medical checks. We know there is often a short period of worry until further checks are done. Knowing that this is a possibility before the test is important, so you can try not to panic.
Do mammograms overdiagnose cancer? Overdiagnosis means we might diagnose an early cancer through screening, but that cancer might never have grown enough to be life-threatening. Some cancers are very slow growing, also some women will be diagnosed with DCIS (ductal carcinoma in situ), this is a very early breast cancer where the cells are abnormal but it is not yet spreading into the surrounding healthy tissue. For younger women overdiagnose is less of an issue. We expect women in their 40’s and 50’s to have many decades ahead so even a slow growing cancer has a long time to cause issues and we should try to diagnose cancers early. Older women may be more at risk of overdiagnosis, we often recommend that annual checks may not be needed at older ages.
Mammograms are slightly uncomfortable. To take an accurate image the breasts are placed between two plastic plates which slightly flatten the breast tissue. Thankfully it only takes a few minutes for the pictures to be taken.
Modern mammogram machines use a low dose of radiation, approximately the same as people would naturally exposed to 7 weeks of normal life.
Do you know your breast density?
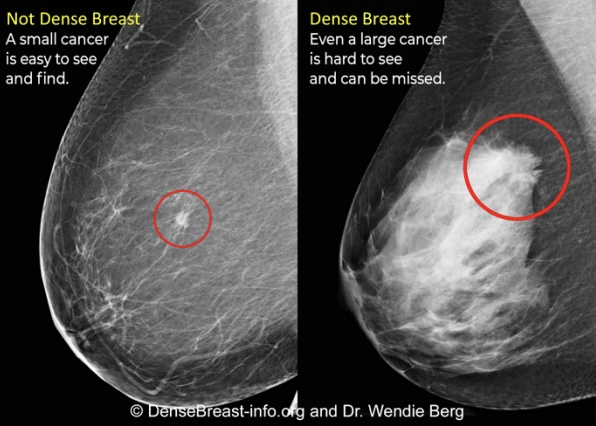
Breast density refers to the make-up of the breast tissue, specifically how much is made up of fatty tissue and how much is ‘denser’ fibroglandular tissue. It matters because we know if you have the highest rating of breast density, category D, it means you are 4 times more likely to develop breast cancer than those in category A.
About 10% of females will have the highest category D density on their mammogram screening. It is important to note that breast density can only be seen on a mammogram, it is not the same as feeling you may have ‘lumpy’ breasts for instance.
Dense breast tissue appears white on a mammogram, this makes it very hard to see breast cancers for women in group D. The USA and France now routinely assess breast density on mammograms. If the result is category D then supplemental imaging is offered with an ultrasound or breast MRI scan. At Coyne Medical, we agree that women should be told their breast density so they can make an informed choice on their screening.
If you are having a private mammogram in the UK please make sure they are assessing your breast density and ask your doctor if you might benefit from extra screening. Currently, the NHS is not routinely assessing breast density, there are many doctors and patients who are trying to change this and hopefully, it will change in the coming years. You can ask your NHS clinic about your breast density. If you’re interested in learning more about Breast Density then do take a look at Dense Breast Info, a brilliant resources for patients and doctors.
🔬 Inherited Risk Factors for Breast Cancer
- About 5-10% of breast cancers are directly caused by an inherited genetic mutation. This means the person has inherited a ‘fault’ in a gene. linked to breast cancer risk from either parent. You might also hear this called a ‘gene mutation’ or ‘pathogenic variant’. Key genes involved include:
- BRCA1 & BRCA2 – High risk: these cause a high risk of breast cancer, for example people with a BRCA1 mutation may have up to 90% lifetime risk of breast cancer.
- PALB2, TP53, CHEK2, ATM – Moderate risk: mutations in these genes carry a 15-60% lifetime risk of breast cancer. The exact estimate will depend on the mutation, as well as other lifestyle factors.
- CDH1, PTEN, STK11 – These are much rarer gene mutations which are associated with breast cancer risk.
🧬 How Do Inherited Gene Mutations Lead To Breast Cancer
Cancers develop when individual cells become faulty. They develop errors in their DNA code which allow them to grow uncontrollably. This lets them become a cancer or ‘tumour’. The cancer can then grow bigger and eventually spread to other parts of the body.
Errors happen in DNA of our cells often. Damage to our DNA is more common as we get older. It also can happen due to other harmful forces such as tobacco smoke and UV radiation. When this happens the body has in-built mechanisms to repair the damaged DNA. There are many different processes and proteins involved in repairing DNA damage.
BRCA1 is a gene which produces BRCA1 protein. This plays an important role in repair DNA damage, it’s called a ‘tumour suppressor’. Everyone has two copies of the BRCA1 gene. One inherited from each parent. If you inherit a BRCA1 mutation from a parent it means the BRCA1 protein that gene makes will not work as well. Therefore it won’t be as good at repairing DNA damage. Over time this means it is more likely your cells will become damaged enough for them to become a cancer.
🧐 Who Should Get Genetic Testing for Inherited Breast Cancer?
We believe everyone can benefit from genetic testing to personalise their cancer prevention and early detection.
Genetic testing is strongly recommended for those who have extra risk of gene mutations.
- A personal or family history of breast cancer, especially before age 50.
- Multiple cases of breast or ovarian cancer in close relatives.
- Jewish ancestry, particularly Ashkenazi Jewish, due to a higher prevalence of BRCA mutations.
- A known mutation in the family (e.g., BRCA1, BRCA2, PALB2).
At Coyne Medical we offer testing for everyone.
The NHS offers genetic testing for high-risk individuals. If you would like to check if you are eligible then speak to your NHS GP. They will ask your details of your personal and family history. You may be sent a questionnaire to complete, knowing when and at what age family members were diagnosed is useful. They will work out the chance of you having a mutation in a breast cancer gene such as BRCA1. If your risk is above the threshold for NHS testing you may be offered a consultation and test.
Why Men With A Family History Of Breast Cancer Should Consider Testing
Half of the people with a BRCA1 or 2 mutation, will be biological males. Many men don’t worry about a family history of breast cancer but this is a mistake.
- Breast Cancer: Men with a BRCA1 or 2 mutation have an increased risk of male breast cancer
- It’s important they regularly check their chest and report any changes or lumps.
- Male breast cancer is generally rare, affecting less than 0.02% of men, if they have a BRCA1 or 2 mutation that jumps to 7-9%.
- It is strongly recommended that any male who has breast cancer themselves have genetic testing.
- Prostate Cancer: They have an up to 60% chance of getting prostate cancer in their lifetime. That’s over 8 times the average male.
- Regular screening such as PSA tests can help them detect this earlier.
- We also have newer screening options available at Coyne Medical, including the Stockholm3 test.
- Pancreatic Cancer: The risk of this cancer particularly affects men over 50 years.
- Men with a BRCA1 or 2 mutation have over 7 times the risk of an average male.
Protecting The Next Generation
When a male relative finds out they have a BRCA1 or 2 mutation for instance they can share this information with family members. This means that their female relatives such as daughters and grand-daughters can potentially be prevented from having cancer.
Many men take great comfort knowing they have helped to safeguard the health of their family.
Not Just Breast Cancer: How Other Cancers Can Be Linked
We know that many of the genes linked to breast cancer are linked to other cancers. So people with family history of these cancers should consider genetic screening. Plus if we find a gene mutation we can then think about how to reduce their risk of cancer and detect it early.
- Ovarian cancer
- Prostate cancer
- Pancreatic cancer
- Melanoma skin cancer
There are links to other less common cancers too including Fanconi’s anaemia.
🛠️ Why More People Should Have Genetic Testing
Genetic testing was once limited to those with a strong family history due to high costs and accessibility issues. However, this approach misses nearly 50% of individuals with a gene mutation.
Many people are unaware of their family history, especially if relatives passed away at a young age. Some families with mostly male members may not show a pattern of breast cancer cases, despite carrying high-risk mutations.
By increasing access to genetic screening, we can shift the focus towards prevention rather than late-stage detection. As Dr. Mary-Claire King states, “To identify a woman as a carrier only after she develops cancer is a failure of cancer prevention.”
We know that less than 5% of people in the UK who have a high-risk mutation such as in BRCA1 have been diagnosed. We passionately want to help change that by getting more people to think about genetic testing.
📊 What Happens Next After Your Genetic Screening Result
✅ Positive Result: Knowledge Is Power
- A positive result means the test did find a gene mutation that increases breast cancer risk.
- We can use your genetic screening result with other information such as your family history and lifestyle to create a personal risk estimate for you.
- Next steps: You may be recommended to have extra screenings or other measures to reduce your risk and detect cancer earlier.
- The good news is that knowing your result does give you the power to make sure you detect cancer early and even prevent it completely.
- For example, women with a BRCA1 mutation will be offered extra screening from the NHS will annual mammograms and MRI scans from 30 to 50 years of age. They can also take medication which can reduce the risk of breast cancer by up to 50%. Some women may choose to have a risk-reducing mastectomy, this surgery removes breast tissue, usually followed by a reconstruction. Risk-reducing mastectomy can reduce the risk of breast cancer by over 95%.
- The good news is that knowing your result does give you the power to make sure you detect cancer early and even prevent it completely.
- At Coyne Medical we will support you every step of the way in getting the best care.
❌ Negative Result:
- No harmful mutations were detected in the tested genes.
- This does not eliminate all breast cancer risk. It is still important to look at your other risk factors to reduce your chance of cancer. This is especially the case if you have a strong family history.
- You can still benefit from cancer screenings. Think about what options you would like to take up through the NHS or privately.
Newer Options To Detect Breast Cancer Early
We can now also use a blood test to find breast cancer earlier, when treatment is often easier and more successful. At Coyne Medical we offer a Multi Cancer Early Detection blood test, called Trucheck Intelli. It uses a simple blood test to look for tumour cells which have broken off from a cancer in the body. It can find cancers before symptoms appear, even at stage 1. It is generally suitable for people aged 40 and over, who have not been previously diagnosed with cancer. Some people aged 35 to 39 can also have the test if they are in a high risk group, e.g. due to having a family history or a gene mutation.
Dr Lucy discovered her own inherited breast cancer risk through genetic screening.She's passionate about giving more people the power of prevention through personalised screening.
Visit Us At Our Clinic in London For The Full Range of Screening Options
🤝 Support & Resources
If you have concerns about hereditary breast cancer, these support groups and resources can provide guidance and community:
- The National Hereditary Breast Cancer Helpline – Provides support for those at risk or affected by hereditary breast cancer.
- BRCA1 & 2 and High-Risk Support Group UK (Facebook) – A community for those with BRCA and other high-risk gene mutations.
- PALB2 Warriors (Facebook) – A group dedicated to individuals with PALB2 mutations.
- Breast Cancer Now – A leading UK charity offering information, support, and research funding.
- Jnetics – a charity dedicated to prevention and diagnosis in the Jewish community in the UK.
